I last wrote about the Dexcom Continuous Glucose Monitor (CGM) on 11 December, 2017. In that post, I highlighted what it was like after a week. The first week was not without hiccups, and the following few weren't perfect either. Things have improved dramatically after almost two months of wearing a CGM. The idea behind this post is to share things I've learnt that weren't obvious from the beginning. These are the things that had I known in December, would've made the first few weeks with the CGM a lot smoother. Your mileage may vary, but this is a collection of what has been working for me.
Overnight
Get your overnight blood sugar level right. That is the single best piece of advice I can give. The biggest annoyance I had with the CGM after a week was the alarms - especially overnight. There's no such thing as perfect control, and things are going to go wrong, but if you can stabilise the night as much as possible, it'll make your life easier. If you've got a CGM, chances are you're controlling your blood sugar levels through an insulin pump. It's important to fine-tune your basal insulin to a rate that will keep you steady overnight. Easier said than done, of course, but if it works 5 or 6 nights per week, you'll be well on your way to having an easier time with the CGM. Being woken three nights a week is no fun for anyone.
But how? Before getting a CGM, I would've told you that it was impossible to have consistent levels overnight. I've since learnt this isn't true. I noticed a correlation between the nights I had stabilised my blood sugar level before sleep (i.e. Was hovering at a constant level, and had no active insulin - this was key). Short-acting insulin stays in your system for just over three hours, so it's important to avoid eating carbs up to three hours before sleeping. I've changed habits to have dinner finished by 7 pm at the latest so that insulin is out of my system by 10 pm. Now I know that if by 10 pm my blood sugar is between 5 & 7 mmol/L, it's unlikely to fluctuate, thanks to no active insulin, and a good basal rate. The result? Hours of uninterrupted sleep. For the sake of your sanity, especially when it comes to alarms that can't be turned off, you'll want to ensure this stability. You may need to tweak basal insulin rates, but it's well worth the effort.
A stable night is advantageous for two reasons; it gets the day off to a good start and helps your average BGL for that day. If my average is higher than usual towards the end of the day, there's a good chance that a bad night was a contributing factor. Ultimately, the goal of using a CGM is to have better stability and control of your blood glucose, which shows in HbA1c results. If the first 6-8 hours of your day are spent at a healthy blood glucose level, that will go a long way to improving your HbA1c.
Bolus early, bolus often
The second most important piece of advice I can give is to bolus (or inject, if needles are your thing) well in advance of eating a meal. Something you'll likely notice during the early days with a CGM is the delay between giving insulin and when it takes effect. If you give insulin for food at the time you begin to eat, you'll see that the food takes effect well before the insulin does, resulting in a spike in your BGL, followed by a dip 60-120 minutes later as the bulk of the insulin takes effect. I've found that giving insulin 20-30 minutes before a meal is the best way to avoid this spike. Your mileage may vary, but I haven't had to worry about my blood sugar falling too fast when bolusing up to half an hour before a meal. Any earlier would put you at risk of a hypo before the food takes effect, so I don't recommend it. Avoiding this spike will not only make you feel better but will help stabilise your blood sugar after eating. The idea is that you then consume food around the time the insulin starts to act in your system, and they balance each other out. It's never perfect, but it may be the difference between "spiking" to 9 mmol/L rather than 13 mmol/L. Avoiding these higher blood sugar levels a few times a day will undoubtedly benefit your HbA1c result.
It's easy to bolus early when you know what you're going to eat at a prepared meal such as an at-home dinner. Eating lunch at uncertain times at work, or eating out and not knowing what to expect can make this quite difficult. You can't bolus 30 minutes in advance of a meal when you don't know what time you'll get around to eating, nor can you bolus correctly for a meal you've never seen before - as is the case when you eat at a restaurant. Years of diabetes management has taught me to guess the carbohydrate content of meals at a glance. Apply this skill to a plate of food you haven't seen before, and you might be able to guesstimate carb quantity in advance. For example, it's a safe bet that a plate of pasta will have a non-zero amount of carb, whereas fish and veggies will have very little carb. In the case of the former, I'd be looking to bolus early for approximately 50% of the carbs I expect in the pasta. A typical bowl might have 50g worth of carb, but as you don't know the portion size, nor when the meal will arrive, I don't recommend bolusing for the full 50g in advance. It's unlikely a bowl of pasta will have <25g, data-preserve-html-node="true" so start by bolusing for that in advance. When the meal arrives, you can use your amazing carb-guessing skills to deliver insulin for the rest of the meal. This has been working for me. Again, it might be different for you. Don't bolus early if your BGL is low to begin with, or if your BGL tends to drop right after bolusing. In my case, I know that if I give insulin for 25g carb, I can afford to wait 30 minutes before eating and still avoid a hypo. It's not always practical to bolus in advance, and that's okay. It isn't the end of the world - after all, it's what you've been doing for years, isn't it? If you're not confident guessing the carb content of a meal in advance or bolusing in advance of eating, you can either choose low-carb food to avoid a spike or just enjoy the meal and accept that a spike now and then is a part of having diabetes. Just be sure to check in with your BGL a few hours later and correct if need be.
Carbs
The next thing I wish I knew is that carbs are bad. Actually, carbs are great. But carbs are bad for your blood glucose levels. You might've read the section above on sleeping and thought, "That's great, but it isn't possible for me to avoid eating within three hours of sleeping." That's fine! Just be more careful with what you choose to eat. You'll quickly realise the types of foods in your diet that need to go. Have a low (or no) carb dinner if you can. Different foods affect different people in different ways, but these are some key things I've learnt:
- Plain Weet-Bix (a cereal with effectively no sugar [~2.5%]) and low-fat milk will send my blood sugar soaring immediately after breakfast. It is classified as a medium-GI food.
- Protein shakes have also been cut out entirely, despite there being no sugar in the protein powder itself. 200mL of milk and a small scoop of ice-cream is enough to raise sugar levels fast.
- Low-GI bread is a lifesaver. Two slices of Lo-GI bread from Bakers Delight has replaced Weet-Bix as my breakfast, and this has a noticeably positive impact on my blood sugar. I rarely spike after breakfast, and if I do, it's to ~9mmol/L, instead of 14mmol/L.
Choosing low-GI foods where possible will help to stabilise your blood sugar levels as these foods release energy slower over a longer period, which is more aligned with how insulin acts in your body. I'd also recommend not eating too much carbohydrate in a short space of time, as it's harder to guess carb content and the effect it'll have on your body. Ideally, you won't see a noticeable spike in your blood sugar after eating, but the ideal is rarely possible. The next best thing is to minimise the spike, and that can be done through a combination of giving insulin early enough, not overeating carbs, and choosing low-GI food.
The sensor
There are a few things worth noting about the sensor itself that would've been handy to know from the beginning.
- The Dexcom CGM sensor is meant to last seven days. I've had it last for less time and fail to give readings (fortunately Dexcom were great about this and offered a replacement), but also considerably more - up to 14 days. I don't suggest leaving it in longer the recommended seven days, but note I had success the one time I tried it. I've only been able to try it once as often the tape has started to peel after 5 or 6 days, so the sensor is ready to be removed on day 7.
- If you're inserting the sensor in your stomach, it's most likely that the top of the tape (closest to your chest) will peel first, so when fixing the tape, I'd recommend sealing the top edge first to ensure it's stuck in place.
- Inserting the sensor doesn't hurt, so don't be afraid. This is a case of do as I say, not as I do - years of changing insulin pump sets has me conditioned to expect pain far too often. Surprisingly, the Dexcom sensor insertion is completely painless. There's only been once where I've found it more noticeable than a tickle, but even then it couldn't be felt after a few minutes. The insertion device is quite large and can be intimidating, but it isn't as painful as it seems.
Sanity (check)
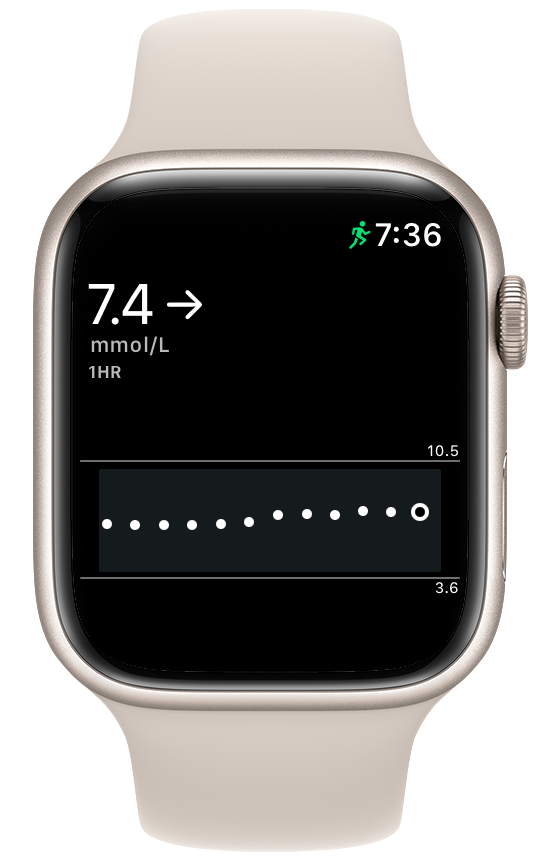
I'm the first person to praise the convenience and luxuries afforded by having an Apple Watch. The potential of the Apple Watch as a health and fitness device is truly unlimited. A long-term hope is that the Apple Watch can perform non-invasive blood glucose monitoring, but until that day we've got invasive solutions. Dexcom's integration with both iOS and watchOS is impressive. The apps are reliable, and that's exactly what you want from a medical device. The Dexcom app for Apple Watch supports a "complication" - this means it's possible to view your blood glucose reading in real-time on the face of your Apple Watch, with no need to open the watch app to see this data. At first, I thought there could be no better feature. After a while, I realised it's unhealthy to be glancing at my watch every five minutes to get an update on my blood glucose level. Focusing on this constantly, and anxiously watching it rise or fall, is no good for anyone. You survived up until now without such frequent updates, so you'll be okay to hide the complication. Opening the watch app every hour or so should still be enough for you to see significant benefit from wearing a CGM without going insane. Again, this is a case of do as I say, not as I do. I'm a lot better at not constantly checking my watch than even this time last month, but it's still more of a distraction than I'd like it to be.
Take a break
Continuous glucose monitoring is, on the whole, fantastic. That doesn't mean it isn't overwhelming at times. There have been many occasions where I've thought it's more trouble than it's worth. Since, things have settled down mainly thanks to bolusing early, and trying to get my levels stable before sleeping. If you feel overwhelmed, I encourage you to take a few days off from wearing it. A great time for this is in between taking out the sensor and putting in a new one. There's nothing wrong with going back to doing things the old way for a while. Sure, your levels might spike, but that's been happening for years, and at least you won't be anxious as you watch your BGL climb after a meal. You'll know when you're ready to put it back in. CGM has more of a learning curve than beginning to use an insulin pump does, and like an insulin pump isn't a device for everyone.
Learning experience
Everything mentioned thus far is something that I've learnt from experience with the CGM. It's only been a couple of months, and I'm sure that the learning will continue to be plentiful for a long time to come. Ultimately the best way to know what works for you is to try yourself. Things won't work perfectly at first. I could not have imagined how frustrated I would be by the alarms after a few weeks of wearing the Dexcom.
What I'd like to see
I'm looking forward to an update to the Dexcom Apple Watch app which brings the ability for the Dexcom to send data directly to an Apple Watch. Currently, your phone must be in range of the Dexcom to receive updates, which are pushed from the phone to the watch. As of watchOS 4, it is possible for a Bluetooth health device to send data directly to the Apple Watch, and Dexcom have said they will support this feature.
I'd also really like to see granular control of the alerts. There's a lot that could be improved here, including:
- Make it clear that by acknowledging an alarm in the iOS app, it will be silenced. I spent days thinking it was impossible to silence alarms, and that I was stuck with being woken every five minutes until my blood sugar rose high enough to stop the alerts.
- Time of day settings. Living in constant fear that your phone will sound an uncontrollable alert is no fun. People have occasions where they don't want to be alerted to things - at work, in meetings, at the cinema, etc. Silent alerts are possible for all but critical low alerts on the Dexcom. This is a start but not perfect, as you then have to remember to turn them on again or else you won't be alerted when you actually want to be - such as overnight. Almost 17 years of diabetes means that if I'm awake, I can tell with 99% accuracy that my blood sugar is low or high. How high, or how low? Who knows, that's what the Dexcom (and previously, finger-pricks) are for, but if I'm awake I'll be able to feel the onset of low or high blood sugar. I'd love to be able to tell the Dexcom to send audio alerts between 10 pm and 6 am, but no other time. Silent notifications to my Apple Watch and iPhone will suffice the other 16 hours of the day.
- To extend on the above, there's the concept of "Low" blood sugar in the Dexcom app. This value is defined by the user (I have mine set to 3.7mmol/L), and anything under this reading will trigger an alert. There's also an "urgent low" alarm - set to 3.1mmol/L - which can't be changed, nor silenced under any circumstances. It's a long shot, and there are other things which should be a priority, but I'd like to see smarter use of these settings based on a wake-up alarm. For example, I absolutely should be alerted to a level of 3.6mmol/L at 2 am. However, if my BGL drops to 3.6mmol/L at 5:30 am, and the Dexcom knows my alarm is set to go off in the next 30 minutes, the fact that the low isn't "urgent" means it doesn't need to wake me. I have no issue with it waking me at any time if the level is considered an urgent low, of course. This is simply something I'd like, and I realise everyone would have a different preference.
- On a similar note, a true wildcard feature would be integration with a sleep tracker on the Apple Watch (AutoWake?). This could mean that if your blood sugar was low and steady, but not falling nor urgently low, it would wait until the end of a sleep cycle to wake you. Let me tell you, Dexcom shows no mercy and will wake you 40 mins after falling asleep if it has to. That is not a time one would want to be woken if it can be avoided.
Again, these business rules are tricky to decide, and this is no easy task to tackle, but in a world where Dexcom have infinite time and resources to develop their mobile apps, I'd like to see it happen. As a general rule, fewer app settings are better, but not for a medical device like the Dexcom, which plays such an important role in the life of the wearer. Fine-grain control is exactly what's needed here, and I find the existing control over alerts to be frustratingly limiting.
Conclusion
Continuous glucose monitoring can benefit every person with diabetes in a slightly different way. For a young child who may not have yet developed the ability to detect low blood sugar, CGM does this for them. For that child's parents, they can send their child off to school knowing that the CGM will catch irregular blood sugar and alert the child sooner than a teacher might notice the child's pale face and scattered concentration, which are both indicators of low blood sugar. For someone my age, CGM is about the freedom and flexibility of not having to carry a blood glucose monitor everywhere I go, but more importantly, it's about smoothing the fluctuations in my blood sugar levels leading to better control which will (hopefully) mean fewer complications from diabetes later in life. For someone prone to fainting when their blood sugar falls, CGM is about saving their life, be it overnight, or just one afternoon while excitedly watching the footy and not realising their BGL has dropped. CGM has infinite potential to benefit people with diabetes, as well as those without it. Learning what works best for each individual takes time, and is no small task. Had I known the tips above this time two months ago, I would've had a much easier time using a CGM in the beginning, and I hope that someone new to using CGM finds the tips to be beneficial.